The term myoarthropathy of the masticatory system refers to a large number of pathologic conditions affecting the masticatory musculature and/or the Temporo-Mandibular Articulation (TMA).
The complexity of this subject matter can be guessed by the wide range of terms used over the years to point out the alterations of the masticatory system, creating further confusion in a field characterized by an interesting and wide multiplicity of nuances1,2. Nowadays, the term Temporo-Mandibular Disorder (TMD) is generally used.
It includes all the alterations connected to the function of the entire masticatory system. Recently, epidemiological studies indicate that around 60% of the total population shows myoarthropathy symptoms.
In particular, the prevalence of symptoms seems to be around 59%, while the prevalence of signs reaches almost the 80% of the total population.
This high prevalence highlights a clear picture of their wide spread diffusion, although this is certainly due to the inclusion, in many scientific works, of signs and symptoms of little importance3-11.
The Michigan splint is a removable appliance frequently used in the treatment of patients with TMD and related diseases, such as tensive headache.
The aim of the present study is to assess the effectiveness of a new protocol built up to relieve pain with pharmacological treatment of chronic TMD, compared to the traditional occlusal therapy protocol by Michigan splint without effective pharmacological therapy.
Materials and Methods 35 patients were enrolled in this study, 21 women (40 ± 10 years old) and 14 men (30 ± 5 years old), who were diagnosed for TMDs; clinical criteria were palpation-related pain and clicking or limited mouth opening.
The clinical diagnosis of TMDs was based on a patient symptom questionnaire including intra-oral and extra-oral muscle examination (Figure 1). All patients were examined by the same investigator in order to avoid any kind of bias.
Furthermore, all subjects signed an informed consent form confirming their voluntary participation in this study. During the objective exams, all patients referred spontaneous and palpation-related pain (Figure 2).
|
Figure 1. Palpation of the masticatory muscles. |
Figure 2. Magnetic Resonance of the TMA of a patient before our therapy. |
Used Drugs Delorazepam Delorazepam (Chlordemethyldiazepam) is a long acting benzodiazepine with anxiolytic, hypnoinducing, myorelaxant and anticonvulsant activities.
It is considered a short-acting benzodiazepine drug which exerts both therapeutic and adverse effects linking with high affinity to GABAA receptor sites in the central nervous system12 enhancing the effects of GABA at the GABAA receptor increasing the opening frequency of its chloride ion channel resulting in the therapeutic benzodiazepines actions13.
Thiocolchicoside Thiocolchicoside is a muscle relaxant with anti- inflammatory and analgesic effects. It acts as a competitive GABA-A receptor antagonist and also inhibits glycine receptors with similar potency and nicotinic acetylcholine receptors to a much lesser extent. It has powerful convulsant activity and should not be used in seizure-prone individuals.
It is a natural glucoside of colchicum without curare-like effects. Thiocolchicoside does not alterate voluntary motility and does not interfere with respiratory muscles. It has no valuable effects on the cardiovascular system.
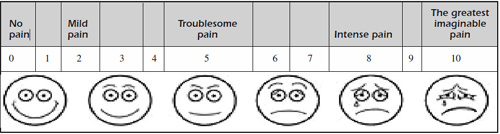
Instrumental examinations were performed by panoramic X-ray (OPT) and magnetic resonance of the TMA. A visual-analogue scale (V.A.S.)14 was used in order to evaluate the intensity pain referred by patients consequent to palpation (Table I).
The first group (treated group = 19 patients) received an occlusal therapy with “Michigan resplint” (Figure 3) and pharmacological therapy with “delorazepam drops” and “thiocolchicoside tablets”.
|
Table I. Visual-analogue scale. |
|
|
Figure 3. Michigan splint |
Figure 4. Magnetic Resonance of the TMA of the same patient after our therapy. |
The second group (placebo group – 16 patients) received occlusal therapy with “Michigan splint” and “Placebo” administration: tablets and drops, prepared by a pharmacist, were similar to those used in the first group, but without the active drugs.
Patients were asked to express their pain intensity marking a point on a straight line, whose left limit was 0 (corresponding to absence of pain) and right limit was 10 (corresponding to the greatest imaginable pain).
The VAS data were collected at T0 and after 6 (T1), 12 (T2) and 18 months (Tmax) from the beginning of treatment. Data collected from the experimental group treated with “Michigan splint” and “delorazepam and thiocolchicoside” were compared with data collected from experimental group treated with occlusal therapy and “Michigan splint” alone.
Furthermore, regarding the occlusal therapy, patients were asked to wear their splint overnight along the first 12 months, positioned on superior arch.
About the pharmacological therapy, the daily dose used were:
-
Delorazepam drops, 1 mg/day (12 drops/day) along 12 months, decreasing 1 drop every month up to 1 drop/day during the whole 12th month;
-
Thiocolchicoside, 1 tablet 4 mg/12 hours along 12 months. Soon after the 12 months treatment, all patients were asked to gradually discard their splint not wearing it on Sunday in the 1st week, Sunday and Wednesday on the 2nd week, Sunday, Tuesday and Friday on the 3rd week, Sunday, Tuesday Thursday and Saturday on the 4th week and wearing it only on Sunday for the next 2 weeks.
The remaining period of time (6 weeks) was considered necessary for a full wash-out from pharmacological treatment. Statistical Analysis V.A.S. data were statistically evaluated using Unpaired t-test. Analysis of variances was further performed with a nonparametric test. Results Comparisons between VAS values of the two experimental groups (Unpaired t-test) before to begin the treatment, gave not significant results (p=0.2990) (two-tailed p=0.6479, t=0.461; df=33) allowing us to proceed. VAS values of the two experimental groups were further compared: At 6 months from the beginning of the treatment, the comparisons between VAS values of the two experimental groups gave the following results: (two-tailed p<0.0088; t=2.785; df=33); F test comparing variances gave no significant results (F=1.739; DFn=18; Dfd=15; n.s.); At 12 months from the beginning of the treatment, VAS data comparisons gave significant results (two tailed p<0.0001; t=7.728; df=33); F test comparing variances (F=3.343; DFn=18; Dfd=15; p<0.0112); At 18 months from the beginning of the treatment, VAS data comparison also gave significant results (two-tailed p<0.0001); t=9.041; df=33). F test comparing variances (F= 4.754; DFn=18; Dfd=15; p<0.0019).
Some patients regularly using the Michigan splint (28 patients=80%) declared it comfortable. Due to the progressive dose reduction, none of the treated patients showed benzodiazepine tolerance signs. In conclusion, the effectiveness of these two types of therapies was assessed by analyzing the V.A.S. data into a statistical view: data comparison between the 2 experimental groups showed a significant improvement or disappearance of the pain only at 12 and 18 months after the beginning of the experiment (p<0.0001).
Discussion Among the large number of splints previously proposed, the “Michigan-type occlusal splints” are the most worldwide used appliances15. Michigan splints are numbered among the centric relation splints. They are characterized by a flat and smooth occlusal surface with a canine guidance on protrusion and laterotrusion. Therefore, a smooth guide surface has been built only in the canine area, in order to allow a 1mm disclusion around the posterior teeth on lateralization and on protrusion.
The remaining part of the occlusal surface remained smooth and plain: this was fundamental to allow the proper mandible to place again into its physiological position. The expected actions of this widely used occlusal appliance are: Increase of the vertical dimension; Reduction of the tone of the mandibular elevator muscles; Removal of occlusal interferences; Reduction of parafunctional movements; Unquestionable placebo effect.
Thanks to these actions, the “Michigan-type occlusal splints” results to be effective in reducing asymmetry of muscle activity, muscle fatigue and all related signs and symptoms of cranio-mandibular disorders.
From the results of our study, it emerged that our non invasive management program of combined therapy is effective in treating painful muscular and related symptomatology restoring the normal parameters of the articular function (Figure 4).
Concerning the occlusal therapy and placebo, our protocol, based on the combination of occlusal (Michigan splint) and pharmacological therapy (delorazepam and thiocolchicoside) is significantly more effective (in the management of joints pain) in those patients in which a self-limiting characteristic of the TMD pathology showed a relevant problem. TMD is a clear example of clinical status commonly dubbed as multifactorial pathologies.
In the past occlusal problems, they were considered the only cause of this type of disorders but a lot of recent studies have definitely proven the impossibility to find an univocal relationship between causes and effects12,13.
Clarity about proper etiologic factors is still a long way off. Nevertheless, there is a common understanding about the identification of some factors which could be included either among the predisposing factors, the causative factors or the perpetuating factors. It would be a mistake to draw up a list of factors and mechanically include them in each one of these categories, as each factor may be a causative factor in a patient, a perpetuating factor in another and neither of them in another one.
Factors with a potential etiologic role are: female gender, depression and anxiety, parafunctions, occlusal disorders, emotional and physical trauma, accidents (especially whiplash injury), posture disorders, hip dysmetria, scoliosis, arthrosis, cervical lordosis16-20.
The therapeutic approach to myoarthropathies is symptomatic rather than a causal one, due to a series of distinctive characteristics of the pathologies under discussion, such as: etiologic complexity and difficulty to identify the causative factors and the intense involvement of the psychosocial sphere. TMDs are pathologies which generally end up in a good prognosis. In many cases there is a spontaneous recovery and most patients report a marked improvement of symptoms thanks to an undertaken conservative, non-invasive management. It is also important to make an accurate and well-timed diagnosis, in order to prevent a chronic developing of such a problem.
Conclusions
This latter chronic condition involves a more complex background, often leading to the necessity of a multidisciplinary approach, including: patient’s assurance and information, acquirement of self-control techniques, physiatric treatment, occlusal therapy, specialists assistance in pharmacotherapy and cognitive-behavioural therapy.
The aim of these therapies is to relieve the most important and recurring symptoms, especially pain and function improvement as well as the quality of life which, in some cases, could be ruined by these annoying disorders, even in daily life activities.
This pilot-study showed that the Michigan splint, combined together with our pharmacological protocol, could improve the predictability in the treatment of the TMD-related pain without a clinical relapse into the following months.
Autors
F. INCHINGOLO, M. TATULLO, M. MARRELLI, A.M. INCHINGOLO, A. TARULLO, A.D. INCHINGOLO, G. DIPALMA, S. PODO BRUNETTI1, A. TARULLO, R. CAGIANO
References
-
STOHLER CS. Phenomenology, epidemiology and natural progression of the muscular temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1997; 83: 77-81.
-
TURK DC. Psychosocial and behavioural assessment of patients with temporomandibular disorders: Diagnostic and treatment implication. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1997; 83: 65-71.
-
POVEDA RODA R, BAGAN JV, DÍAZ FERNÁNDEZ JM, HERNÁNDEZ BAZÁN S, JIMÉNEZ SORIANO Y. Review of temporomandibular joint pathology. Part I: classification, epidemiology and risk factors. Med Oral Patol Oral Cir Bucal 2007; 12: E292-298.
-
COOPER BC, KLEINBERG I. Examination of a large patient population for the presence of symptoms and signs of temporomandibular disorders. Cranio 2007; 25: 114-126.
-
CASANOVA-ROSADO JF, MEDINA-SOLÍS CE, VALLEJOSSÁNCHEZ AA, CASANOVA-ROSADO AJ, HERNÁNDEZ-PRADO B, AVILA-BURGOS L. Prevalence and associated factors for temporomandibular disorders in a group of Mexican adolescents and youth adults. Clin Oral Investig 2006; 10: 42-49.
-
PALLA S. Mioartropatie del sistema masticatorio. In: Mioartropatie del sistema masticatorio e dolori orofacciali. RC libri, Milano, 2001; pp. 1-36.
-
SIEBER M, PALLA S. Lo stress come causa di mioartropatie – In: Mioartropatie del sistema masticatorio e dolori orofacciali. RC libri, Milano, 2001; pp. 37-50.
-
ERNST B, GALLO LM, PALLA S, CHEN YJ. L’articolazione temporomandibolare nella rappresentazione per immagine. In: Mioartropatie del sistema masticatorio e dolori orofacciali. RC libri, Milano, 2001; pp. 251-290.
-
ISLER H. Cefalee: Diagnosi differenziale. In: Mioartropatie del sistema masticatorio e dolori orofacciali. RC libri, Milano, 2001; pp. 327-336.
-
PALLA S. Principi di terapia delle mioartropatie. In: Mioartropatie del sistema masticatorio e dolori orofacciali. RC libri, Milano, 2001; pp. 349-388.
-
Barbalonga E, Catalano S, Doglio P, Ferrero M, Gilardi G, Macaluso GM, Morani V, Preti G, Sedran A. Aspetti funzionali e morfologia occlusale. In: Riabilitazione protesica. UTET, Torino, 2003; pp. 51-98.
-
MATTHEW E, ANDREASON P, PETTIGREW K, CARSON RE, HERSCOVITCH P, COHEN R, KING C, JOHANSON CE, GREENBLATT DJ, PAUL SM. Benzodiazepine receptors mediate regional blood flow changes in the living human brain. Proc Natl Acad Sci USA 1995; 92: 2775-2779.
-
RISS J, CLOYD J, GATES J, COLLINS S. Benzodiazepines in epilepsy: pharmacology and pharmacokinetics. Acta Neurol Scand 2008; 118: 69-86.
-
INCHINGOLO F, TATULLO M, MARRELLI M, INCHINGOLO AM, PICCIARIELLO V, INCHINGOLO AD, DIPALMA G, VERMESAN D, CAGIANO R. Clinical trial with bromelain in third molar exodontia. Eur Rev Med Pharmacol Sci 2010; 14: 771-774.
-
KIRVESKARI P. The role of occlusal adjustment in the management of temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1997; 83: 87-90.
-
MANFREDINI D, CHIAPPE G, BOSCO M. Research diagnostic criteria for temporomandibular disorders (RDC/TMD) axis I diagnoses in an Italian patient population. J Oral Rehabil 2006; 33: 551-558.
-
POVEDA RODA R, BAGAN JV, DÍAZ FERNÁNDEZ JM, HERNÁNDEZ BAZÁN S, JIMÉNEZ SORIANO Y. Review of temporomandibular joint pathology. Part I: classification, epidemiology and risk factors. Med Oral Patol Oral Cir Bucal 2007; 12: E292-298. JOHNSON AL. Temporomandibular joint litigation: resolving issues of medical necessity and contract ambiguity. Semin Orthod 1997; 3: 128-132.
-
AKHTER R, HASSAN NM, AIDA J, KANEHIRA T, ZAMAN KU, MORITA M. Association between experience of stressful life events and muscle-related temporomandibular disorders in patients seeking free treatment in a dental hospital.Eur J Med Res 2007; 12: 535-540.
-
LIN YC, HSU ML, YANG JS, LIANG TH, CHOU SL, LIN HY. Temporomandibular joint disorders in patients with rheumatoid arthritis. J Chin Med Assoc 2007; 70: 527-534.