Arnold-Chiari malformation type I is a genetic malformation related to the reduced structure of the posterior cranial fossa, which contains the brainstem and cerebellum. With the size of the posterior fossa too small, they herniate through the foramen magnum and into the spinal cord.
Since the nervous system needs the cerebrospinal fluid to flow freely through the craniocervical junction and the entire spinal cord, the cerebellar tonsils protrude into the cervical spinal canal and block the flow of the fluid, with possible brain damage.
In this malformation, both the lower part of the spinal column and brain are completely normal. The only defect is the underdevelopment of the occipital bone, which cause the herniation of cerebellar tonsils due to the overcrowding of nervous structures in the posterior cranial fossa.
Nuclear magnetic resonance (NMR) can show the reduced flow and its speed in the central nervous system, more specifically in the cisterna magna and subarachnoid spaces.
CASE REPORT
A 23-year-old Caucasian male patient with Arnold–Chiari malformation type I. He was born from dystocic delivery and non-consanguineous healthy parents. The genetic test showed chromosome deletion in the following locus: (1), (q23.1q31.2).
Due to this chromosome abnormality, the patient developed psychomotor retardation with cranial dysmorphism, hypoplasia of the corpus callosum, Arnold–Chiari malformation type I, multifocal leukoencephalopathy and congenital antithrombin III deficiency.
|
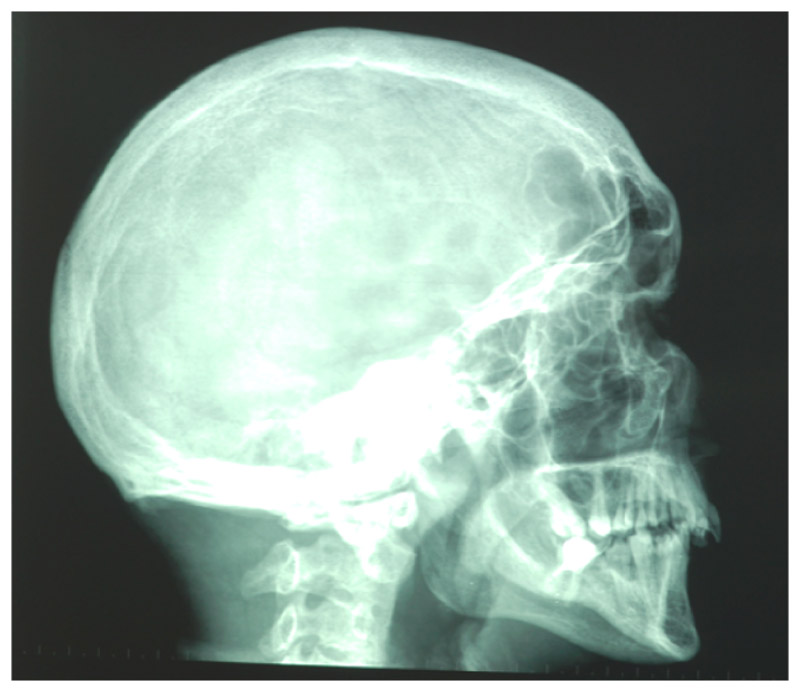
1. Latero-lateral projection teleradiography |
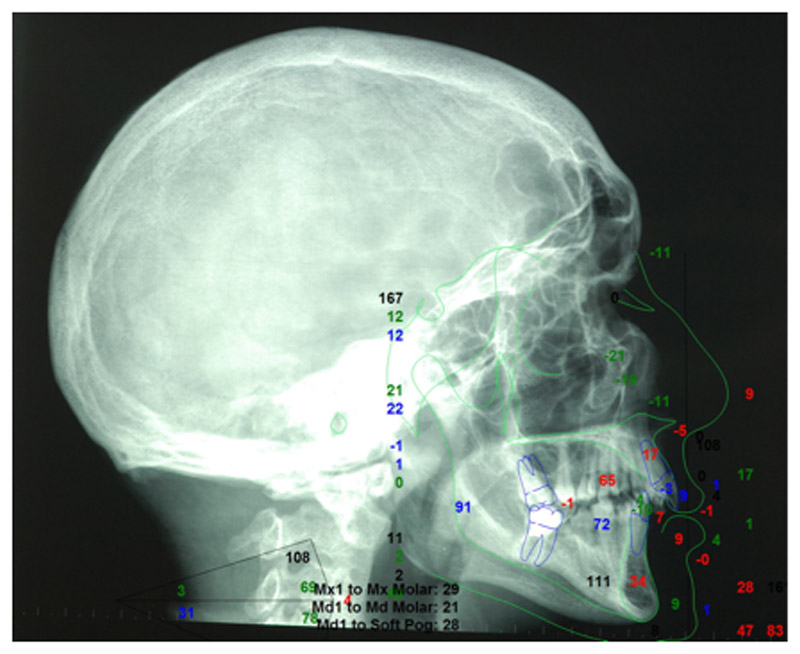
2. Cephalometric analysis |
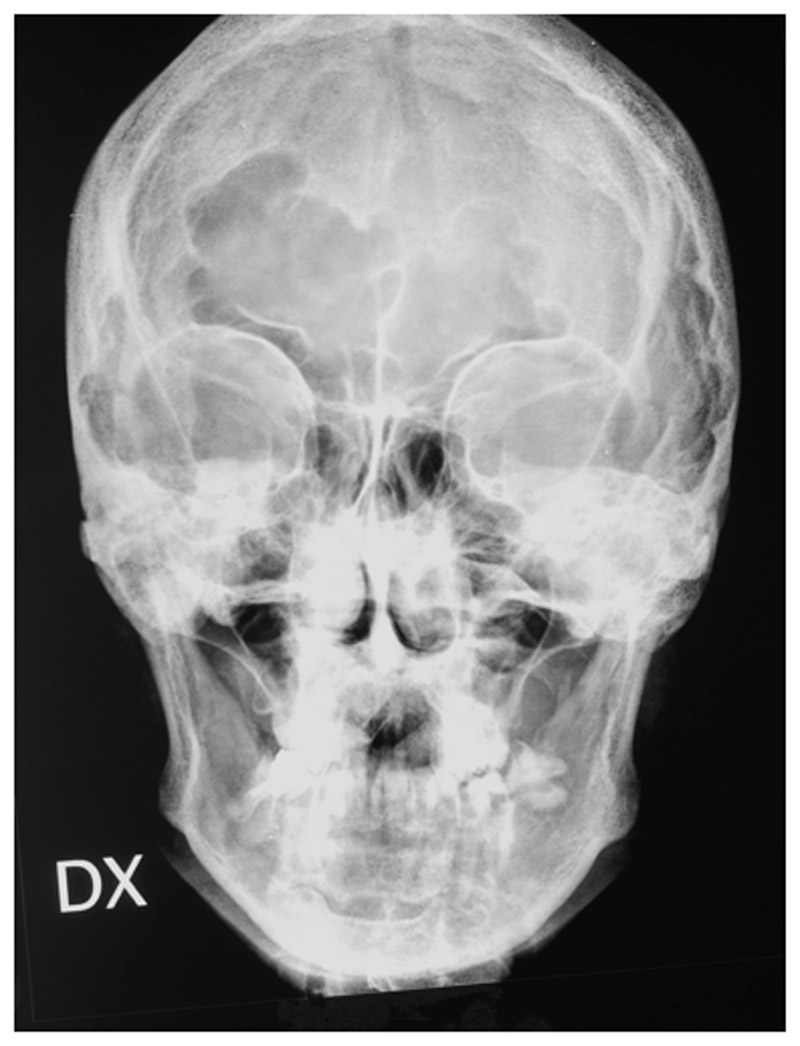
3. Posteroanterior projection x-ray |
CEPHALOMETRIC STUDY
All radiologic tests were performed to establish the syndromic diagnosis: encephalon NMR, x-ray of chest, hand and wrist, EEG, ECG.Our study focused on the cephalometric analysis of the patient’s facial skeleton. Besides, rhinomanometry was necessary for the diagnosis of oral respiration.
– Skeletal and dental Class II malocclusion (ANB=63°; WITS appraisal=3.7 mm),
maxillomandibular biprotrusion (SNA=95°, SNB=88.7°) with sagittal overdevelopment of the upper jaw.
– Slight facial hyperdivergence (FMA=36°) caused by prevalent increase in lower facial divergence (occlusal plane^mandibular plane 33.6°). The occlusal plane is rotated counterclockwise (PP-OP 2.9, MP-OP 30.7°).
– The inclination and position of the upper incisor is practically normal, with a slight tendency to inward inclination; inward-inclined lower incisor
– Arnett soft tissue analysis confirms the maxillomandibular biprotrusion, with overjet increase (Mx1-Md1).
– Facial height shows a mild lip incompetence caused by lower lip length deficiency. Total facial height is reduced (na’-me’ 82.8 mm) due to the reduction of the lower facial third.
– Reduced thickness of soft tissues of the chin and lips.
– Projections on True vertical line confirm the maxillomandibular biprotrusion and indicate an insufficient mandibular body projection (NTJ-Pog’).
Congresso Nazionale dei Docenti di Discipline Odontostomatologiche e Chirurgia Maxillo Facciale
Firenze – Siena, 14-16 Aprile 2011
Università degli Studi di Bari Dipartimento di Odontostomatologia e Chirurgia
Direttore: Prof.ssa D. DE VITO
Calabrodental S.r.l. Unità Operativa di Chirurgia Maxillo-Facciale Regione Calabria – Crotone Dir. San: Dott. M. W. Marrelli
AUTHORS
CARBOTTI F. * ; INCHINGOLO F. ; DIPALMA G. ; DE CAROLIS M. ; MARRELLI M. ; INCHINGOLO A. D. ; PALLADINO A. ;CAGIANO R. ; ; INCHINGOLO A. M. ; FAGGIANA F. ; ANGELINI V.
BIBLIOGRAFY