Gingival hyperplasia is an increase in volume of the gingival tissue, together with an increase in the number of cells.
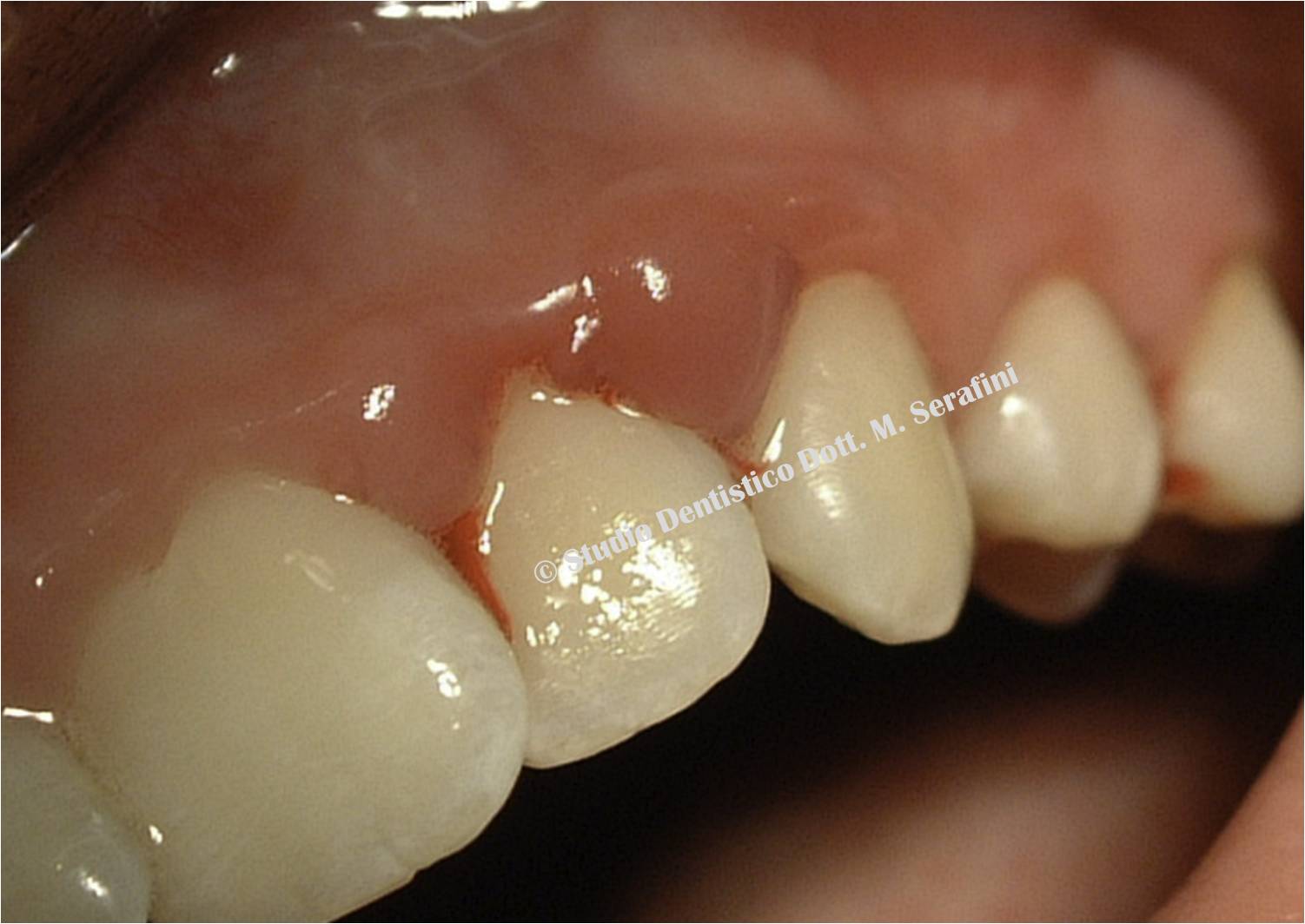
The gingiva is reddish or red-bluish, with an increased size both in coronal and bucco-lingual direction. Several etiologic factors are responsible for localized gingival hyperplasia: it can be classified from a topographic and ethiopatogenetic point of view.
The therapy varies according to its origin and nature: it ranges from etiologic therapy, which is the removal of the irritating stimulus, like in inflammatory hyperplasia, to surgical therapy.
The aim of the present study is to show the advantage of using laser therapy in the treatment of a 14-year-old female patient, presenting with a reddish gingiva and bleeding on probing in the upper maxilla. Around the teeth number 13 – 23 there was a deep-red sessile mass, characterized by easy bleeding.
The diagnostic hypothesis was epulis, but there was no histological confirmation so it was identified as gingival hyperplasia.
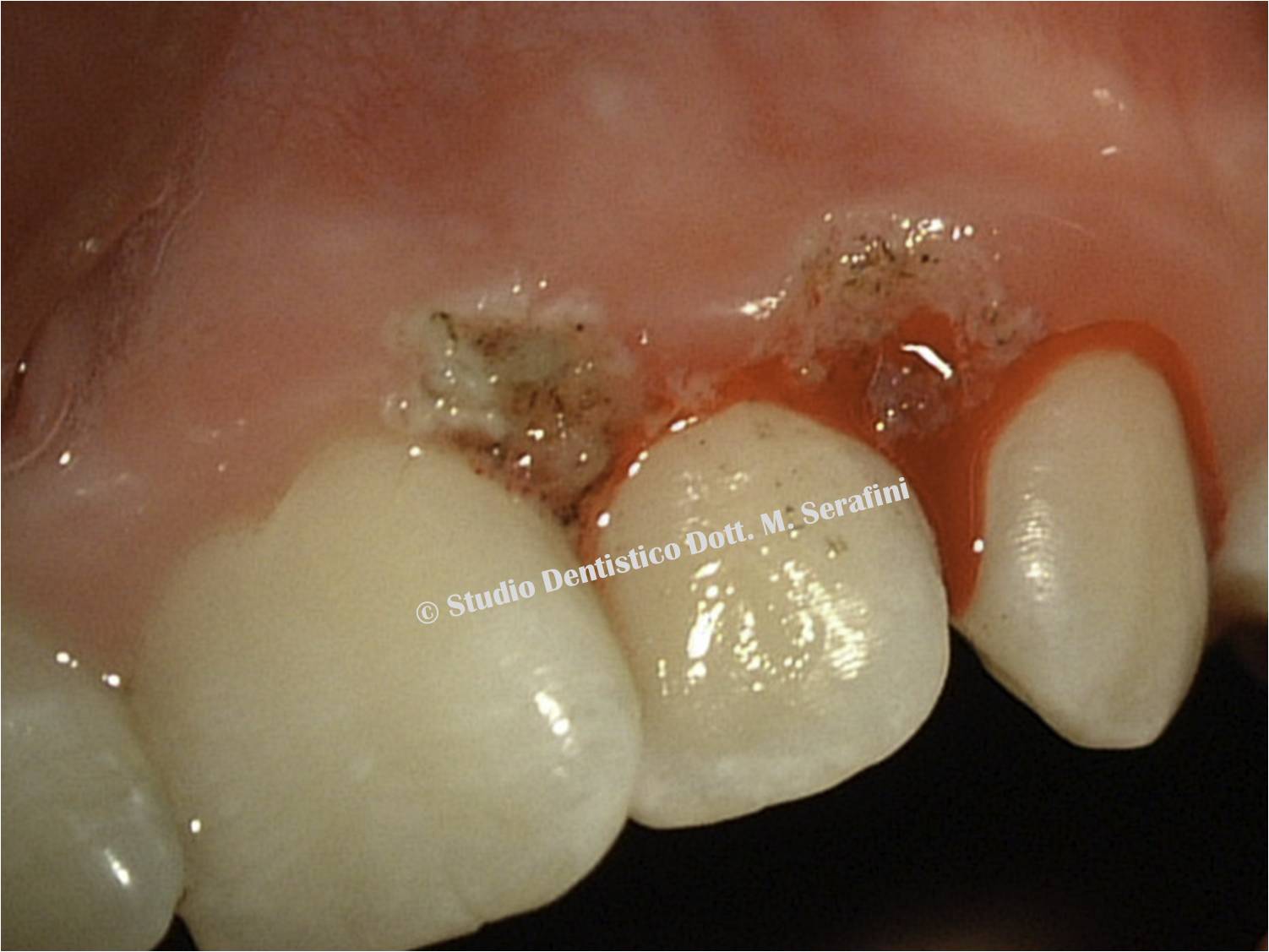
We performed an initial preparation (hygienic phase), revaluation, surgical therapy and maintaining phase. After initial treatment, which consisted in plaque control, surface scaling, root planing and polishing, the clinical examination showed the permanence of an increased gingival volume which caused masticatory disorders.
Hyperplastic tissues were removed with laser therapy, which proved advantageous because it was painless for the patient, did not require anesthesia and gingival incisions, and provided better hemostasis.
After 15 days, the objective clinical examination revealed perfect healing of gingival lesions.
|
Congresso Nazionale dei Docenti di Discipline Odontostomatologiche e Chirurgia Maxillo Facciale
Firenze – Siena, 14-16 Aprile 2011
Università degli Studi di Bari Dipartimento di Odontostomatologia e Chirurgia
Direttore: Prof.ssa D. DE VITO
Calabrodental S.r.l. Unità Operativa di Chirurgia Maxillo-Facciale Regione Calabria – Crotone Dir. San: Dott. M. W. Marrelli
AUTHORS
F. Inchingolo, F. Schinco* G. Dipalma, M. Serafini, S. Di Teodoro, A. M. Inchingolo, M. De Carolis, M. Marrelli, A. Palladino, A. D. Inchingolo
REFERENCES
2. N Escudero-Castaño, M.A Perea-García, J Campo-Trapero, Cano-Sánchez, and A Bascones-Martínez. Oral and Perioral Piercing Complications. Open Dent J. 2008; 2: 133–136.
3. Ziebolz D, Stuehmer C, van Nüss K, Hornecker E, Mausberg RF. Complications of tongue piercing: a review of the literature and three case reports. J Contemp Dent Pract. 2009 Nov 1;10(6):E065-71.
4. Kapferer I, Berger K, Stuerz K, Beier US. Self-reported complications with lip and tongue piercing. Quintessence Int. 2010;41:731-737.
5. Hickey BM, Schoch EA, Bigeard L, Musset AM. Complications following oral piercing. A study among 201 young adults in Strasbourg, France. Community Dent Health. 2010 Mar;27(1):35-40.
6. Pires IL, Cota LO, Oliveira AC, Costa JE, Costa FO. Association between periodontal condition and use of tongue piercing: a case-control study. J Clin Periodontol. 2010 Aug 1;37(8):712-8. Epub 2010 Jun 17.