Peri-implantitis is a physiological process affecting the soft and hard tissues surrounding the peri-implant unit and causing loss of osseointegration and bone support. It is associated with bleeding, often with suppuration, and it is considered as the implant equivalent of periodontal disease. Several studies showed that the application of diode laser and Er:YAG laser, also in combination with Clorexidine, is extremely effective in the decontamination of the implant surface in case of bacterial peri-implantitis.
AIM
The aim of the present study is to clinically demonstrate the potential of antimicrobial photodynamic therapy of peri-implantitis.
MATERIALS AND METHODS
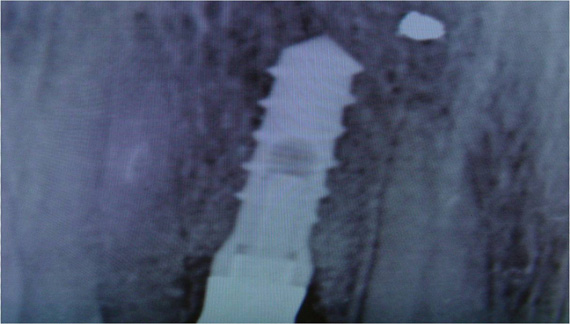
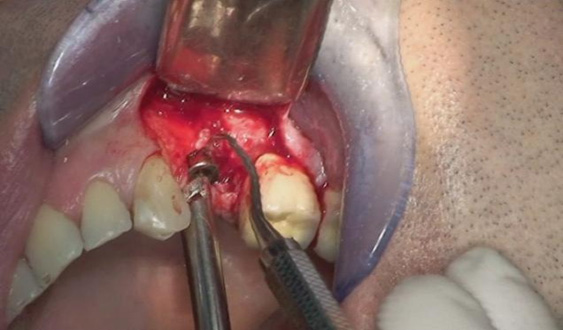
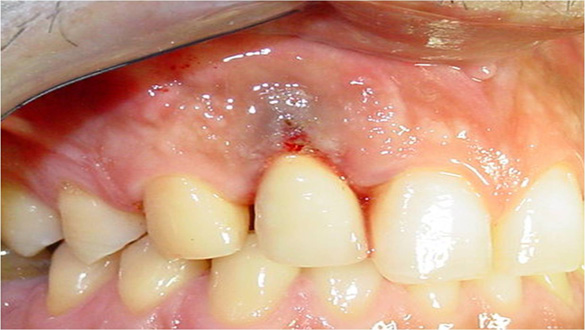
Two patients affected by severe peri-implantitis were selected to evaluate the improvement of their clinical conditions after photodynamic therapy. The clinical data were collected before treatment and 6 months after treatment. Before treatment, both patients presented with local pain on percussion, Probing Attachment Level (PAL) >3 mm, bleeding index = 2 (BOP+), peri-implant radiotransparency, Periodontal Probing Depth (PPD) >5 mm.
The first patient was treated with diode laser while the second patient was treated with Er:YAG laser. Both treatments were performed after infiltration of local anesthetic with vasoconstrictor and after mechanical removal of peri-implant granulation tissue. In addition to laser therapy, the second patient received regenerative therapy with micro-granules of heterologous bovine bone (Bio-oss) and Bio-Gide membrane, since a greater area of osteolysis could be observed around the implant.
RESULTS
The 6-month follow-up revealed that all the parameters under consideration obtained a statistically significant improvement with both types of treatment. No pain, negative BOP, no suppuration, PAL <2 mm, PPD <3 mm, no mobility, reduced radiotransparent area of osteolysis indicating an increased osseointegration.
DISCUSSION AND CONCLUSIONS
Diode laser, if used with the right parameters, provides effective decontamination of the implant surface. To this day, any risks associated with the increased temperature and/or with the ultra-structural modifications of the implant and its surrounding structures can be excluded.
The micro-explosions induced by Er:YAG laser can effectively remove the surface of titanium dioxide from implants affected by peri-implantitis.
Excessive overheating of the treated area, caused by Er:YAG laser irradiation, can be avoided with the use of saline spray, which protects the surrounding bone tissues and increases the chances for an osseointegrated implant.
These results clearly show that the problems arising from the treatment of peri-implantitis can be successfully solved with the use of diode laser and Er:YAG laser.
Università degli Studi di Bari “A. Moro” Dipartimento di Odontostomatologia e Chirurgia
XX Congresso nazionale Docenti di Odontoiatria
AUTHORS
F. Inchingolo, G. Malcangi, M. Marrelli, A. Palladino, M. Tatullo, A.M. Inchingolo, F. Schinco, A.D. Inchingolo, L. Burdo, G. Marinelli, G. Dipalma, G. Paduanelli, N. Tempesta
BIBLIOGRAFY
Bach G, Neckel C, Mall C, Krekeler G.: “Conventional versus laser-assisted therapy of periimplantitis: a five-year comparative study”. Implant Dent. 2000;9(3):247-51 Heitz-Mayfield LJ. “Peri-implant diseases: diagnosis and risk indicators. “J Clin Periodontol. 2008 Sep; 35(8 Suppl):292-304 Kreisler M et al. “Effect of Nd:YAG, Ho:YAG, Er:YAG,CO2, and GaAlAs laser irradiation on surfaces properties of endosseus dental implants.” J Oral Maxillofaccial Implants, 2002:17: 202-211 Romanos G, Nentwig G. “Diode laser (980 nm) in oral and maxillofacial surgical procedures: clinical observations based on clinical applications. “ J Period 2000;71:810-5.